Like I’ve mentioned in a few of my previous posts, this pandemic has brought on a lot of changes for everyone– but there is variation in how COVID-19 has impacted different groups of people. The experience of racial and ethnic minorities during this pandemic has been very different from other groups and is reflective of health outcomes that often exist for minorities in the U.S.
COVID-19
In New York City, the death rates for Black/African American individuals is much higher due to the virus, than it is for other racial/ethnic groups (1). The chart below shows the disproportionality of the effects of COVID on the population of African American individuals in a few states. 
Compared to the total state population, the majority of patients affected by COVID are African American (2).
These disparities exist not only during this pandemic, but in healthcare in general: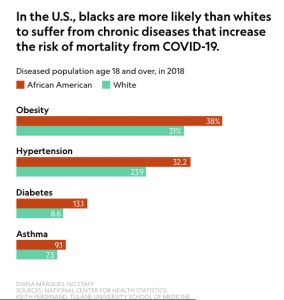
Reasons for the Disparity
People who belong to racial or ethnic minority groups experience the health care system differently than others– many of the existing disparities in society lead to poorer health outcomes, as well as greater vulnerability to viruses and other illnesses. Many minority groups live in heavily populated areas or live in households with multiple generations, where social distancing might not be possible (1). Many work hourly, so health benefits are not part of the package and health services become difficult to access (2). There is also a much higher population of racial and ethnic minorities in jails, prisons, etc. which are again, places that increase the risk of spread of viruses and other illnesses (1).
Also, because of the social distancing measures that have to be taken because of the pandemic, there has been a decrease in quality of care for patients who don’t speak English (4). Before, interpreters/translators could be present in person during a patient’s visit, which makes it much easier to translate and understand the patient’s concerns and symptoms. Now, a lot of interpreters have to work over the phone and it’s possible that a lot of information is getting lost in translation because it’s just harder to have a conversation and understand each other that way.
While the pandemic has affected everyone in one way or another, it has not affected everyone equally. The social determinants of health that I talked about in my first blog, in addition to factors such as racism, geographic location, and poverty, play a large part in deciding how an individual is affected. Unfortunately, the same level and quality of healthcare are not available to every person. Moving towards a system that addresses these disparities and provides excellent health care to each patient will involve first resolving the inequalities that exist in health care delivery in general and access to healthier food, exercise, etc. Additionally, training healthcare providers to better understand cultural differences and barriers to care could improve health outcomes for minority groups (3).
