Currently, a large portion of the world is still being affected by the scary and deadly virus that is COVID-19. As of right now, we are approaching the 10-month mark since the reporting of the first US case in Washington State. Unfortunately, it seems like the number of COVID-19 cases is beginning to rise once again.
Although I live in Houston, TX, I study at Union College located in Schenectady, NY. I, along with everyone else at my school, was obligated to leave campus immediately after the school had its first confirmed COVID-19 case on March 12th. There was a wave of anxiety and fear that spread amongst everyone. I flew back home on March 15th after packing up all of my belongings, finding last-minute storage, and switching my spring break flight to a sooner date. I remember arriving in Houston at around 2 am completely exhausted. I felt an immediate sense of relief once I saw my parents and embraced them as we knew things were beginning to get worse in NY. Soon NY became the epicenter of the COVID-19 pandemic. Since my flight on March 15th, I have remained at home.
 Today, November 11th, I woke up to a headline that stated that Texas is now officially the first state in the US to surpass 1 million COVID-19 cases, a devastating new record. Experts claim that the US is entering the “worse period” since the onset of the pandemic as there has been a week-long streak of 100,000 daily cases and record hospitalizations. You would think that things would be getting better by now but, from the data, it seems to me that the US is losing its grip on the pandemic once again. It is evident that things are becoming much more difficult to control as people are tired of being stuck indoors. I know I am but, regardless of this, my health and that of my family is a priority to me. Focusing back on Texas, Harris County (where Houston is located) ranks first amongst all other Texas counties when it comes to the number of COVID-19 cases. An article in Independent, claims that if Texas was a country, it would be ranked the 10th highest amongst other infected nations. Yikes!
Today, November 11th, I woke up to a headline that stated that Texas is now officially the first state in the US to surpass 1 million COVID-19 cases, a devastating new record. Experts claim that the US is entering the “worse period” since the onset of the pandemic as there has been a week-long streak of 100,000 daily cases and record hospitalizations. You would think that things would be getting better by now but, from the data, it seems to me that the US is losing its grip on the pandemic once again. It is evident that things are becoming much more difficult to control as people are tired of being stuck indoors. I know I am but, regardless of this, my health and that of my family is a priority to me. Focusing back on Texas, Harris County (where Houston is located) ranks first amongst all other Texas counties when it comes to the number of COVID-19 cases. An article in Independent, claims that if Texas was a country, it would be ranked the 10th highest amongst other infected nations. Yikes!
Action Taken at a State Level (March- July):
 I have compiled a few of what I believe are important points, announcements, declarations, orders, headlines, etc. and organized them chronologically. I use this approach to demonstrate the response to the COVID-19 pandemic over time in relation to health care and to my community. I will begin by mentioning that the first case was announced in Texas, more specifically in the Greater Houston area, on March 4th.
I have compiled a few of what I believe are important points, announcements, declarations, orders, headlines, etc. and organized them chronologically. I use this approach to demonstrate the response to the COVID-19 pandemic over time in relation to health care and to my community. I will begin by mentioning that the first case was announced in Texas, more specifically in the Greater Houston area, on March 4th.
On March 10, Governor Greg Abbott and the Texas Department of Insurance (TDI) announced that they asked health insurers and health maintenance organizations to waive costs associated with testing and telemedicine visits needed for the diagnosis of the virus. This was an effort to ensure no Texan is denied access to testing resources. A few of the specific requests made included requesting insurers to waive co-payments, co-insurance, and deductibles for testing, waive consumer cost-sharing, facilitate telemedicine, cover necessary medical equipment, supplies, and services, and waive penalties restrictions as well as claim denials for necessary out-of-network services.
March 13– Governor Abbott declared a State of Disaster for all counties in Texas. He also promised to “ramp-up” testing and urged that there is no need to panic-buy. At this point, there were more than 30 confirmed cases and over 50 Texans pending test results.
The next day, Governor Abbott directed the Texas Medical Board and the Texas Board of Nursing to fast-track the temporary licensing of out-of-state physicians, physician assistants, certain retired physicians, nurses, and other license types to assist in Texas’ response, all which was now possible due to the State of Disaster declaration. With this, now there was an increasing supply of health care professionals available to provide in-person and telemedicine help across the state. Out-of-state physicians were now able to obtain a Texas limited emergency license or hospital-to-hospital credentialing through this period. Over time, Abbott continued to loosen restrictions on requirements in other areas such as long-term care, pharmacists, and more in an effort to get more hands on deck.
March 17– Abbott held a call with hospital CEOs and representatives across the state to provide updates on care capacities. The Governor and hospitals discussed the supply, staffing, and bed capacities of hospitals to ensure that health care providers have the support they need to assist patients. They were also able to discuss strategies that would further increase these capacities including a temporary waiver for hospitals to increase unused bed capacity without having to submit an application or deal with associated fees. At this point, the state’s COVID-19 count was 64 cases.
On that same day, Abbott waived some regulations for telemedicine. Patients with state-regulated plans could now make telemedicine consultations that would be paid the same way/amount as in-office visits for insurance purposes. Doctors were now eligible for payment from insurance plans regulated by the Texas Department of Insurance for visits conducted over the phone instead of in-person at the same rate they would receive for in-person visits. As a reminder, Texans covered by CHIP or Medicaid would not be charged co-pays for tests or telemedicine consults. Patients that are covered by Medicare or large employer plans still had to check with their own health plan administrators to determine their specific benefits.
March 19– The Commissioner of the Department of State Health Services, John W. Helllerstedt, M.D., issued a Public Health Disaster Declaration.
March 20– Governor Abbott directed the Texas Department of Criminal Justice (TDCJ) to temporarily suspend inmate fees for health care services related to COVID-19. While incarcerated Texans within TDCJ facilities were never denied access to health care due to inabilities to pay, the temporary waiver was implemented to encourage timely reporting of COVID-19 symptoms. The number of cases for the state was now 194 with Harris County being the county with the largest concentration of cases in the whole state (24 cases).
March 21– There is a continued need for health care professionals, more specifically nurses, so now Abbott allowed temporary permit extensions to practice for graduate nurses and graduate vocational nurses who still had not taken their licensing exam. Students who were in their final year of nursing school could now meet their clinical objectives by exceeding the 50% limit on simulated experience and, nurses who were retired or had inactive licenses could now reactivate them.
March 25– Abbott allowed certain health facilities that were still under pending licenses status or had been closed for no more than 36 months to become active under a hospital with an existing license. The was no longer a mileage restriction which allowed hospitals to operate additional facilities that were more than 30 miles away from the main location. This was great because more buildings could now provide space for patients!
April 2- An Executive Order is put in place and it requires all Texans to stay at home except to provide essential services or to do essential things (ex. Go grocery shopping).
April 6– Governor Abbott announces the Care.com initiative to increase in-home child care access for frontline workers. Care.com offered 90 days of free premium access to its services and also provided specific portals for frontline workers in Texas.
April 27– Abbott announced the first phase of a three-phase plan that would “safely and strategically” open up Texas. Under Phase I, certain services and activities were allowed to open with limited occupancy. The Texas Department of State Health Services (DSHS) issued minimum standard health protocols for all businesses and individuals to follow. All retail stores, restaurants, movie theaters, malls, state museums, and state libraries were permitted to reopen starting on May 1st with a limited capacity of 25%. Within shopping malls and museums, the food-court dining areas, play areas, and interactive displays still had to remain closed. Local public museums and libraries had to get permission from the local government. Bars, barbershops, gyms, and hair salons had to remain closed.
May 7th– Oh no, a controversial confinement issue! A Dallas judge sentences a hair salon owner, Shelly Luther, to jail for violating the state’s emergency order on May 5th alongside a $7,000 fine. Public outcry led to Abbott modifying his Executive Order from April 2, eliminating jail time as a punishment for disobeying orders. Barbershops were allowed to open the following day.
May 18– Under Phase II, restaurants could now increase their occupancy to 50%. Additional services and activities that remained closed under Phase I could now open. Bars, child care centers, and other businesses still had to have 25% capacity.
May 29- Protests began to take place in Houston, where George Floyd grew up from the age of 2. This made many people worried about the containment of the virus but many people also believed it was crucial to protest as it was an unjust killing that should not be tolerated. #BlackLivesMatter
June 3– Under Phase III, the final phase, all businesses in Texas could now operate at up to 50% capacity, with very limited exceptions. Businesses that previously have been able to operate at 100% capacity could continue to do so, and most outdoor areas were not subject to capacity limits. This phase was effective immediately. Was this a smart choice? Personally, I don’t think so because the announcement came just one day after the state saw its largest single-day increase in cases since the start of the pandemic. The Office of the Texas Governor even wrote that between May 26th and June 2nd, there were over 45% of new cases coming from jails or prisons, meatpacking plants, and nursing homes. At the moment of Phase III, there were 1,487 Texans hospitalized due to COVID-19, 20,679 active cases, and about 45,858 Texans recovered.
But guess what? The reopening did not last!!
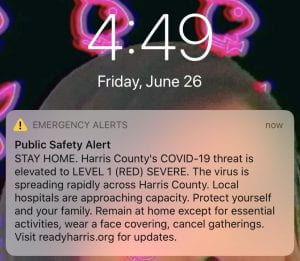 June 26- Abbott rolled back phase III of the reopening strategy and stated that restaurants had to return to 50% capacity from 75% and bars were completely shut down again. That very day, I received a Public Safety alert on my phone alerting me that COVID-19’s threat had elevated to severe for Harris County. Here’s a screenshot I took of the alert 🙂
June 26- Abbott rolled back phase III of the reopening strategy and stated that restaurants had to return to 50% capacity from 75% and bars were completely shut down again. That very day, I received a Public Safety alert on my phone alerting me that COVID-19’s threat had elevated to severe for Harris County. Here’s a screenshot I took of the alert 🙂
July 2– Abbott issued a statewide mask order in counties with 20 or more positive cases. It required people to wear masks when in public. This was a huge step as many conservatives were against the idea of a mask mandate and the governor himself resisted it for months.
What about Houston specifically?
 When people were becoming more informed about COVID-19, only a few expected it to reach the point that we are seeing now. Interestingly enough, as I was doing my research for this blog post, I found an article titled “Why Houston is uniquely situated to be better prepared for the coronavirus threat”. Even though the article was published back in January and there were still no confirmed cases in Texas, the article seemed to claim that if it were to reach Houston, we were going to be more than prepared without really having to do anything abnormal. When reading the article, they kept referring to the coronavirus as a “flu-like virus” which I believe downplays the severity. They also mention the Strategic National Stockpile that apparently is kept in various places around the country as a precautionary measure for a pandemic. The article even boasts the fact that Houston is considered a home to Galveston’s Center for Biodefense and Emerging Infectious Diseases as it is one of only a handful of high-level containment laboratories in the entire country. It is a bit disappointing to see that instead of preparing for the virus, it sounded like many were sitting down thinking nothing big was going to happen in Houston. I believe it’s better to prepare for the worst rather than pretending nothing will happen.
When people were becoming more informed about COVID-19, only a few expected it to reach the point that we are seeing now. Interestingly enough, as I was doing my research for this blog post, I found an article titled “Why Houston is uniquely situated to be better prepared for the coronavirus threat”. Even though the article was published back in January and there were still no confirmed cases in Texas, the article seemed to claim that if it were to reach Houston, we were going to be more than prepared without really having to do anything abnormal. When reading the article, they kept referring to the coronavirus as a “flu-like virus” which I believe downplays the severity. They also mention the Strategic National Stockpile that apparently is kept in various places around the country as a precautionary measure for a pandemic. The article even boasts the fact that Houston is considered a home to Galveston’s Center for Biodefense and Emerging Infectious Diseases as it is one of only a handful of high-level containment laboratories in the entire country. It is a bit disappointing to see that instead of preparing for the virus, it sounded like many were sitting down thinking nothing big was going to happen in Houston. I believe it’s better to prepare for the worst rather than pretending nothing will happen.
When things started to take a turn for the worse, there was significant clash between the City officials in Texas and the State’s government. City officials including Harris County Judge, Lina Hidalgo, a democrat, can be quoted saying that she “had the authority and [She] did require masks in public months ago… We had great compliance because law enforcement would show up and educate and folks would get it”. Hidalgo had issued a mask order on April 22nd but, 5 days later, Governor Abbott used an Executive order to prevent local governments like Harris County from issuing fines even though, at the time, there were more than 25,000 confirmed cases according to an article in The Hill. Because of Abbott’s Executive order, Hidalgo claims that all she is able to do now is issue recommendations.
Steve Adler, Austin’s Mayor, also claimed that Governor Abbott has been saying people should wear masks because it is one of the most important things a person can do right now, yet he took away the authority of cities to impose mandatory mask orders. Consequently, more people stopped wearing protective masks. What this health crisis seems to really emphasize is the constant battle between conservatives who dominate the state legislature and the liberals who run the state’s largest cities, includes the city of Houston.
A Business Insider article also shined a light on the local vs state issues that result from different views on how to control the outbreak. Houston Mayor, Sylvester Turner, blamed Abbott’s decision to strip his authority as the reason the city cases were getting out of control. Houston’s cases skyrocketed in June and July as well as statewide after Abbott reopened the state’s economy on May 1st, “ending one of the nation’s shortest stay-home orders.” Local officials were prohibited from mandating masks and imposing fines for not complying. Turner, along with other Texas mayors teamed up to request Abbott to allow them to put in-place face mask mandates but the idea was dismissed. It wasn’t until 2 weeks later that Abbott issued his one statewide order. Many are angry at the limitations as they know many more lives could have been saved if strict measures were implemented from the beginning. From the beginning, Turner thought Abbott’s idea to reopen was bad and a premature decision. He believed it would simply wipe “away all the gains that [was] achieved”. Turner noted that more Houstonians contracted and died of COVID-19 in July than in March, April, May, and June combined.
When it comes to the great city of Houston, there is already a timeline that is extremely detailed and constantly being updated. This is quite helpful for anyone who wants to know exactly what is going with the pandemic in Houston, TX. The first post of the timeline was made at noon on March 9th and posts have been made practically every single day after that. Some days even have multiple updates! I find the updates extremely reliable as they go in-depth using names, quotes, and statistics all while being appropriately dated and time-stamped. Feel free to check it out in your free time (heads up it’s a long read if you are thinking of checking things out from the beginning). Here’s the link!
Check these resources out!
 Though this blog has been full of information as I wanted to cover the handling of the pandemic from the beginning, I would like to include a few more resources that one could check out and see how the COVID-19 cases are looking in Houston.
Though this blog has been full of information as I wanted to cover the handling of the pandemic from the beginning, I would like to include a few more resources that one could check out and see how the COVID-19 cases are looking in Houston.
Currently, Houston is still a Level 1 (Severe) location even though we are reporting fewer cases compared to June and July. To see Houston’s curve, check out the Harris County/Houston COVID-19 Cases Dashboard. You can tailor the data depending on what you would like to see. Some options are seeing cases by race/ethnicity, zip code, age, sex, etc. Personally, I believe this Vulnerability Map is much cooler and informative. You are able to see much more including the active COVID-19 cases per 10,000 Population. You can input different layers into the map such as “Socioeconomic Social Vulnerability Score”, Health risks such as lack of health insurance, the prevalence of Asthma, the prevalence of smokers, what percent of populations are Black, or what population percentage is Hispanic. A plus to this map is that all layers are depicted in different colors so feel free to overlap them and try to spot out any trends!
Now to end on a positive note, please watch the following inspirational video about Houston. Houston has gone through significant natural disasters yet we have always found a way to unite and prevail together. I am confident when I say we definitely plan to follow this approach to get through the pandemic because we are #HoustonStrong.
Blackman, Jeremy, and Jeremy Wallace. “Gov. Abbott Expands Reopening as Texas Sees Record Number of New Cases.” HoustonChronicle.com, Houston Chronicle, 3 June 2020, www.houstonchronicle.com/politics/texas/article/Gov-Abbott-expands-Texas-reopening-to-50-of-15315307.php.
“COVID-19 Cases by Super Neighborhood – Houston.” ArcGIS Web Application, 2020, mycity.maps.arcgis.com/apps/webappviewer/index.html?id=7424619290f943ef86d68f77fae46f70.
Garcia, Julie. “Why Houston Is Uniquely Situated to Be Better Prepared for the Coronavirus Threat.” HoustonChronicle.com, Houston Chronicle, 27 Jan. 2020, www.houstonchronicle.com/lifestyle/renew-houston/health/article/How-Houston-is-preparing-for-coronavirus-threat-15011416.php.
Hardin, Kristy. “From Harvey and Imelda to Coronavirus- Is Houston Prepared From Past Events?” Versa Creative, 29 Apr. 2020, versacreative.com/blog/from-harvey-and-imelda-to-coronavirus-is-houston-prepared-from-past-events.
“Harris County/Houston COVID-19 Cases.” ArcGIS Dashboards, 2020, harriscounty.maps.arcgis.com/apps/opsdashboard/index.html.
Lamm, Stephanie. “Reopening Texas during COVID-19.” The Houston Chronicle, The Houston Chronicle, 2 Oct. 2020, www.houstonchronicle.com/projects/2020/texas-reopening-covid-timeline/.
Moritz, John C. “Texas Coronavirus Updates: How the State Is Handling the Outbreak.” Caller Times, Corpus Christi Caller Times, 13 Mar. 2020, www.caller.com/story/news/local/texas/state-bureau/2020/03/13/coronavirus-texas-updates-how-state-handling-covid-19-outbreak/5044830002/.
“News.” Office of the Governor | Greg Abbott, 2020, gov.texas.gov/news.
Relman, Eliza, and Rhea Mahbubani. “Houston Mayor Says the City’s Coronavirus Crisis Could’ve Been Avoided If Texas’s Governor Hadn’t Obstructed Local Efforts to Control the Outbreak.” Business Insider, Business Insider, 7 Aug. 2020, www.businessinsider.com/houston-mayor-accuses-texas-governor-of-undermining-coronavirus-effort-2020-8.
Wilson, Reid. “Texas Cities Say State Is Making Pandemic Worse.” The Hill, 27 June 2020, thehill.com/homenews/state-watch/504779-texas-cities-say-state-is-making-pandemic-worse.
Woodward, Alex. “Texas Becomes First State in US to Reach 1 Million Coronavirus Cases.” The Independent, Independent Digital News and Media, 11 Nov. 2020, www.independent.co.uk/news/world/americas/texas-coronavirus-cases-death-toll-b1721137.html.
Wray, DiannaCatherine Wendlandt, and Catherine Wendlandt. “Here’s What You Need to Know about the Coronavirus in Houston.” Houstonia Magazine, Houstonia Magazine, 2020, www.houstoniamag.com/health-and-wellness/what-to-know-about-houston-coronavirus.

























